
19 Jun Medical Respite Care Is Eluding Bay Area’s Black Population

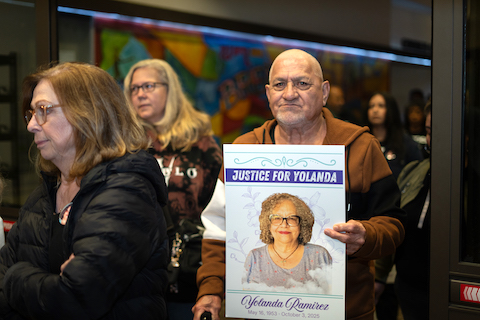
Patrick Smith, 51, in front of his room where he received rehabilitation at Lifelong Adeline Recuperative Care. (Yolanda Taase / LifeLong Adeline Recuperative Care)
By Charles Ayitey
Bay City News
For six years, Patrick Smith wandered the streets of Hayward. The 51-year-old battled drug addiction most of his adult life. It started in his early 20s. Though he overcame the habit, Smith relapsed in his mid-40s. In 2016, his mental health worsened — he had no hospital to turn to for care.
In 2022, Smith’s turning point came when he began rehabilitation at the Herrick Campus of Sutter Health’s Alta Bates Summit Medical Center. After two months of care, Smith was referred to LifeLong Adeline Recuperative Care — a not-for-profit medical center in Oakland providing medical and mental health services to the Bay Area’s underserved homeless population.
“Life is good now,” Smith reflected, saying he has been sober for over a year. “My focus now is to get employment and reunite with my family.”
Smith, a Black man, received medical respite care that many people in the Bay Area can’t access. The National Health Care for the Homeless Council refers to medical respite care as short-term residential care for people experiencing homelessness who are too sick to recover from a physical or mental illness from the streets yet not ill enough to be admitted to a hospital.
Black people in the Bay Area are twice less likely to access medical respite care in their lifetime as compared to white and Latinx people — an issue the NHCHC attributes to limited availability, lack of information, and systemic biases.
>>>Read: Black People More Likely to End Up in Bad Nursing Homes
Alameda County’s 2022 Point-in-Time count of homeless people found that of the county’s homeless population, 43% were Black despite Black people making up only 10% of the county’s population.
“Equity is part of why we are concerned about the social determinants of health,” said Kathryn Boyle, a Kaiser Permanente Northern California project manager. “Understanding that there’s huge health disparities in our communities in terms of access to care, utilization of care, all the way down is crucial.”
The National Institute for Medical Respite Care, a federal initiative to expand medical respite care in the country, said in a press release last year there are 133 medical respite or recuperative care programs nationally, with more than 40 based in California.
Despite this number, there is still a significant shortfall in recuperative care beds compared to the demand — primarily in the Bay Area.
To solve this problem, Kaiser is partnering with local agencies to expand access to medical respite programs across the Bay Area to address the growing homelessness crisis.
“Releasing people to the streets is insane,” Boyle said. “Kaiser’s medical respite care work is building capacity in the community to serve all communities better.”
Since March 2022, Kaiser, a health care provider with many hospitals around the region, joined health nonprofits Dignity Health and the California Health Care Foundation to expand the capacity of recuperative care programs in the Bay Area.
It’s a two-year initiative that ends in 2024. Kaiser’s total investment across all regions is $3.4 million, of which Northern California has contributed $600,000. Through collaboration with the National Institute for Medical Respite Care, Kaiser funds several respite care programs, including at the LifeLong facility where Smith gained sobriety and safe housing.
Smith’s experience at LifeLong was different from what he had expected.
“My initial thought was to rest, get better, and leave,” he said. “But I was given time to rest. It transformed my life.”
Brenda Goldstein, an independent health care consultant at LifeLong, believes that the connection between respite services and homelessness is critical. She argues that homeless individuals — especially Black people — often suffer from higher rates of chronic illnesses and mental health issues worsened by living on the streets.
Goldstein suggests that providing adequate respite care services can improve health outcomes for this population and offer a stable environment that may help them transition into permanent housing.
“The opportunity to stay at respite has been unique and sometimes life-changing for them,” she said, “It’s a chance to pause and heal from whatever health conditions they were in the hospital for or were impacting their well-being while on the streets.”
Private medical respite care providers like LifeLong need help to meet demand. They face financial challenges and high operating costs, limiting their ability to serve needy people. The result? Longer wait times and reduced care access for those who most need it.
“Equity must be at the core of public health,” Goldstein said. “Correcting some of those disparities that have happened over decades and millennia solves these issues in our healthcare system.”
Copyright © 2023 Bay City News, Inc. All rights reserved. Republication, rebroadcast or redistribution without the express written consent of Bay City News, Inc. is prohibited. Bay City News is a 24/7 news service covering the greater Bay Area.




No Comments