21 May Virus Threats Extend Beyond Winter Surge
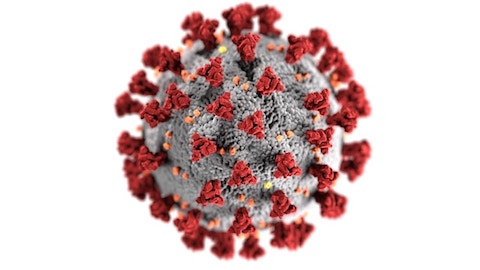
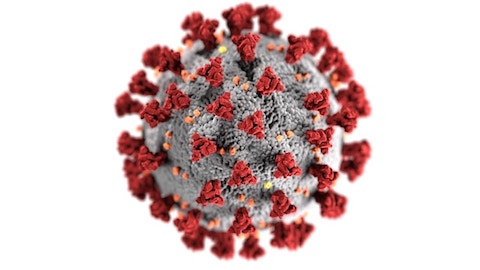
A visual rendering of a coronavirus. (Illustration by CDC on Unsplash)
Editor’s note: This story was written in the days following the news briefing but mistakenly left unpublished. It is produced now to give the writer credit for her work and the information to our readers. Some of the phrasing has been updated.
By America Leon
A host of respiratory viruses arose last winter, presenting considerable national and worldwide public health threats.
In a Jan. 10 Ethnic Media Services news briefing, five infectious disease and medicine experts discussed some of the public health challenges we could encounter this year and how we may be able to mitigate them amid the concern of environmental disasters, political changes, and declining vaccination rates.
Dr. Nahid Bhadelia, founding director of the Center on Emerging Infectious Diseases at Boston University, expressed concern about climate change’s impact on the spread and predictability of infectious diseases. Bhadelia pointed to the potential “secondary impacts” we may see arise from weather-related disasters — such as January’s Los Angeles wildfires — on “medical supplies [and the] use of antibiotics.”
Dr. Peter Chin-Hong, an infectious disease specialist at UCSF, voiced worries about the “anti-science movement,” which has contributed to vaccine hesitancy in recent years.
Undervaccination is a significant issue that will certainly make dealing with viral infections a challenge this year. Dr. Benjamin Neuman, professor of biology at Texas A&M University, spoke about the continuing decline in vaccination rates for non-obligatory vaccines, including the flu shot.
“If you compare the amount [of flu vaccines] that have been delivered this year, it’s 11 million doses less than were delivered by this point last year. Compared to 2020, […] 49 million Americans […] are not vaccinated this year compared to then,” said Neuman.
The Trump administration has presented another cause for concern among public health experts.
We may see “modified” or “lessened” vaccine requirements for children. Neuman explained that school-mandated vaccines have been vital to eradicate “easily preventable viruses” and diseases that “a lot of younger children catch,” including polio.
“If the immunity of the youngest group who are the most susceptible [and] the most likely to spread the viral franchise […] are no longer protected, then I think we’ll see a lot of spillover into older people, parents [and] communities,” said Neuman.
The panel addressed Donald Trump’s indication that he intended to withdraw the United States from the World Health Organization, something he ultimately did on his first day in office this year. Before it happened, Bhadelia said, the move would affect “our ability to be part of the global security framework” through which “countries can participate and share data,” and exiting this “global community” would leave the United States ill-equipped to handle public health challenges that emerge from abroad.
Robert F. Kennedy Jr., now head of the Department of Health and Human Services, has proposed making substantial changes to U.S. health agencies.
At the time of the briefing, there was some uncertainty about whether his alarming propositions would come to fruition, but “if [Kennedy] carries out everything he says, it would gut the infectious disease and research landscape in the United States of America,” said Neuman.
Human metapneumovirus, or HMPV, is a respiratory virus related to RSV that attracted attention due to a highly publicized outbreak in China near the start of the year. However, it is not something the American public needs to be particularly worried about.
Dr. William Schaffner, professor of medicine in the Division of Infectious Diseases at the Vanderbilt University School of Medicine, said that HMPV is well-known to infectious disease and public health experts; outbreaks occur globally each year, and individuals may unknowingly contract it numerous times during their lifetime.
Chinese public health authorities assured that the HMPV outbreak is “within normal limits” for that time of year. Schaffner affirmed that it would not result in a global pandemic.
Regarding the norovirus, Schaffner said that even “very few viral particles” can initiate an infection of this highly contagious intestinal virus, characterized by a few days of sickness, in which individuals may lose fluids through vomiting and diarrhea. People can contract the virus at any time of the year, but it did spike during the winter surge in viral illnesses.
According to Schaffner, the norovirus “can persist in the environment,” spread through close personal contact and be transmitted through food.
Although a norovirus vaccine is in the research pipeline, there is no vaccine available at this time. “Hand hygiene wipes and gels” are ineffective “against the norovirus,” said Schaffner, so washing our hands with soap and water as well as avoiding people who are sick is critical.
A newly identified variant of mpox, Clade 1B, has been regarded as a “public health emergency of international concern” because it “acts more severely than previous types of mpox we have encountered,” said Chin-Hong.
The original strain of mpox, Clade 1, was transmitted primarily through contact with animals. The type of mpox we saw emerge in 2022, Clade 2, was mainly transmitted through sexual contact, existing in “more than 100 countries” and “causing more than 100,000 cases,” said Chin-Hong.
Clade 1B mpox is an “in-between clade” that spreads through direct interaction with animals, sexual contact, and in households. It was present at the time of the briefing “across 12 countries outside of Africa,” and there had been “more than 50,000 cases and more than 1,000 deaths, mainly in children under the age of 15,” said Chin-Hong.
Although experts do not expect an outbreak of Clade 1B mpox in the United States, Chin-Hong emphasized that Clade 2 mpox remains a threat, “still causing hundreds of cases and more in the United States every year.”
One mpox vaccine is available in the United States. The JYNNEOS vaccine is recommended for gay and bisexual me or people who may come in contact with mpox due to their occupation, according to Chin-Hong. A second vaccine exists but is “targeted for Africa right now.”
South America and the Caribbean saw an unprecedented increase in cases of the Oropouche virus. “Brazil, for example, reported about 300 cases a year ago, but this year, it’s more than 10,000 cases,” said Chin-Hong.
Transmission of the Oropouche virus primarily occurs from being bitten by small insects called midges. “However, sexual transmission has recently been identified as a potential way to transmit it,” said Chin-Hong.
Some travel-associated cases of the Oropouche virus have reached the United States; however, the Centers for Disease Control and Prevention reports that “local transmission has not been detected in the United States,” and infectious disease experts do not expect an outbreak this year.
Dr. Maurice Pitesky, doctor of veterinary medicine at UC Davis, discussed the continued threat and impact of avian influenza.
According to Pitesky, avian influenza has reached “six of our seven continents, including Antarctica,” affecting “wild and domestic birds, […] wild and domestic mammals,” in the outbreak that has lasted more than three years.
Pitesky warns that inadequacies in the virus surveillance system for dairy and poultry workers who have “the occupational risk” of exposure to avian influenza may prevent experts from identifying whether the virus evolves to exhibit “the potential for human-to-human transmission” before it spreads significantly.
The threat of COVID-19 also remains, though only “around 8% of the U.S. population has had the [latest] booster,” said Neuman.
The XEC subvariant of COVID-19 is “fairly large, but “seems to be holding steady,” indicating that it will likely be “on the way out,” while strains that are relatives of JN1 and KP3 appear to be rising, “both of which are covered well by the vaccines that are still available,” said Neuman. However, CDC data indicates that LP.8.1 is now the overwhelmingly dominant strain, accounting for 70% of cases in the U.S. from April 27 to May 10.





No Comments