
16 Aug Medi-Cal Eligibility Being Reconsidered for Over 150K in Bay Area

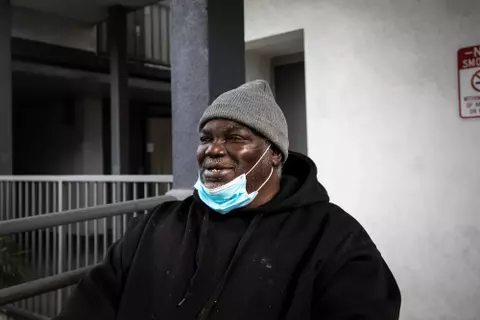
People who lose Medi-Cal eligibility may be able to receive reduced-cost coverage through the Covered California marketplace. (Courtesy of Covered California via Bay City News)
By Lydia Sidhom
Bay City News
About 15.5 million Californians — including over 150,000 people across the Bay Area — will have their Medi-Cal eligibility reconsidered.
As of June, 21% of Medi-Cal recipients in California — or approximately 225,000 people — have lost coverage as a result of the redetermination process, in which needs for the health coverage are reassessed, according to the California Department of Health Care Services.
Termed the “great unwinding,” determining who is still eligible for coverage comes as a response on the federal level to large numbers of people across the U.S. who enrolled in Medicaid, a program designed to provide medical services for low-income individuals with limited resources, to get help during the pandemic.
>>>Read: Medicaid Health Coverage Is Guaranteed, but for How Much Longer?
In late March, states were given 14 months to complete the redetermination process for all Medicaid enrollees.
To keep receiving Medi-Cal, recipients must return a packet of paperwork to their county that is mailed to them for their eligibility to be reassessed. In many cases, individuals have lost access to Medi-Cal for failure to return the packet, according to the DHCS.
Disenrolled recipients, though, are granted until Sept. 30 to return the packet to be reinstated.
In each of the nine counties in the Bay Area, between 60 to 70% of packets that were due were completed, with San Francisco County having the highest return rate and Contra Costa County having the lowest.
Watch Out for Yellow Envelope to Avoid Losing Medi-Cal Coverage
For those who return the packet and are rendered no longer eligible, the state has established a pipeline through Senate Bill 260 that helps people transition from the Medi-Cal plan to reduced cost coverage with Covered California.
The DHCS, as well as clinics and local nonprofit organizations, have launched outreach campaigns that aim to provide information needed to fill out the paperwork. The state has also allocated funds to hire “health enrollment navigators,” individuals designated to be points of contact to help with filling out and returning paperwork.
Out of all Californians disenrolled in Medi-Cal this year, 53% are Latino, according to an advocacy group.
“For us, that figure is too many,” Seciah Aquino, executive director of the Latino Coalition for a Healthy California, an organization that advocates for health equity for California’s Latinx community, said in a media briefing Tuesday.
The main source of confusion for many individuals in this community, Aquino said, is the logistics of filling out forms correctly and returning the packet.
She emphasized that the contact information of navigators and other resources be readily available, and that information be provided in as many languages as possible.
Copyright © 2023 Bay City News, Inc. All rights reserved. Republication, rebroadcast or redistribution without the express written consent of Bay City News, Inc. is prohibited. Bay City News is a 24/7 news service covering the greater Bay Area.



No Comments