08 Jan Medical Experts Weigh In On Trio of Rising Winter Virus Cases
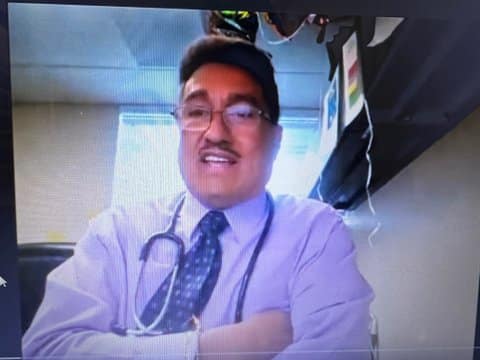
Dr. Jose Perez, chief medical officer at L.A.’s South Central Family Health Center, spoke about the symptoms of multiple viruses during an Ethnic Media Services national briefing on Friday. (Screenshot captured by Joe Porrello / The CC Pulse)
By Joe Porrello
Cases of COVID-19, influenza and respiratory syncytial virus are growing throughout the U.S.
Ethnic Media Services hosted a trio of doctors Friday to discuss prevention and treatment, along with the differences of symptoms and severity for each virus.
Chief virologist of the Global Health Research Complex at Texas A&M University Dr. Benjamin Neuman believes equal precaution should be taken for all three infections.
“It really doesn’t matter which variant you have when you’re laying in a hospital bed or a medically induced coma,” Neuman said. “If any of these gets through your defenses, there is an increased risk of hospitalization and death, and the vaccines mitigate that.”
According to the Centers For Disease Control and Prevention, 29,000 hospitalizations in the U.S. due to COVID-19 took place during a single week in December, with the JN.1 subvariant accounting for about half of the latest cases.
The CDC estimates 14 million cases of influenza with 13,000 deaths in the final quarter of 2023 alone, and between about 60,000 and 80,000 hospital visits annually for RSV cases.
Dr. Jose Perez, the chief medical officer at South Central Family Health Center in Los Angeles, said it is difficult to tell which of the three viruses is affecting a patient based on symptoms alone.
He said people infected with any of the three viruses may experience coughing, sore throat, runny nose, fever and shortness of breath. The viruses also all invade the body through bodily fluids from an infected person and can cause lower respiratory infection, which can lead to bronchitis and pneumonia.
To make diagnosis harder, each of the three viruses can infect an individual simultaneously, according to Perez.
The trifecta of infections see a collective rise in cases during the winter months, sometimes referred to by experts as a “tripledemic.”
Neuman said RSV cases peaked at the end of November, flu cases reached their highest point in mid-December, and that cases of COVID-19 are still rising.
“At every stage in COVID, the virus has done things that are unexpected because this is a new virus, and we’re still learning about what it can do and how it can change, and with each new variant, we learn something new, but we’re always a little bit behind the virus,” said Neuman.
>>>Read: As COVID Variants Outpace Vaccines, We Need to Keep Up
He said JN.1 is growing faster than any other variant and is likely to get into one’s system despite preexisting immunities.
“I think that’s the main reason why it’s concerning,” said Neuman.
According to Neuman, new symptoms for JN.1 include anxiety and sleeplessness.
It takes about seven to 10 days after infection for the virus to grow, incubate, and make you sick, and roughly the same amount of time after symptoms are seen until an individual is no longer contagious, said Perez.
COVID, flu and RSV all cause upper respiratory infections, which Perez said everyone is at risk for.
Taking measures to prevent catching or spreading illness — such as staying six feet away from others, wearing a mask, washing your hands, staying home if you feel sick, and getting vaccinated — is just as important now as ever, Perez said.
The COVID and flu vaccines are available to those six months old or above. Infants eight months or younger, children between eight and 19 months at risk of severe disease, and adults aged 60 or older based on health risk factors are eligible for RSV vaccination.
With the federal government ending the public health emergency declaration in May, vaccines are no longer automatically available for free. Financial responsibility now falls to a person’s health plan, which may include a co-pay.
In California, the Vaccines For Children and Vaccines For Adults programs enable anyone with Medi-Cal health insurance to get the vaccine free of charge through their provider.
Additionally, adults who do not have health insurance or whose insurance does not cover the COVID vaccine can get it for free through the CDC’s Bridge Access Program.
Neuman noted that despite the imperfection of current immunization formulas, getting vaccinated is the best way to defend one’s body from any of the three infections.
“The immune system is made up of a bunch of cells that are really not connected to each other. They just communicate at a distance… Vaccines are really the only way to the entire group of them, which is what you have to do,” he said.




No Comments